
Hospital “Community Benefit” Activities Can Help Expand Access to Nutritious Foods Produced by Strong Local and Regional Food Systems
On May 8, 2015, the Connecticut Food Policy Council convened a state-wide Summit to explore how a new federal regulatory development applicable to tax-exempt hospitals opens opportunities for hospital-community collaboration to strengthen food and nutrition programs and food systems that can prevent hunger and food insecurity.
More than 100 representatives of Connecticut tax-exempt hospitals, public health and social assistance agencies, local farmers markets, urban farmers, and other food system stakeholders gathered at Middlesex Community College to learn more about the final IRS Rule (December, 31, 2014) implementing the Affordable Care Act (2010) provisions mandating that, in order to maintain tax-exempt status, hospitals must comply with a multi-step regulatory framework, every three years, to:
- Assess community health needs using reliable data, with input from public health agencies and community stakeholders,
- Assign priorities to the needs identified, and
- Create and execute an “Implementation Plan” that includes evaluation methods and metrics to addressing the priority needs.
The process is intended to foster continuous quality improvement and requires annual reporting of actual activities and impact, so that every future community health needs assessment and implementation plan builds upon the lessons learned and achievements of the prior cycle.
The final rule makes clear that “significant health needs” are not confined to clinical health care services that hospitals might provide as charity care, but includes social determinants of illness, such as “access to adequate nutrition” that are essential to the health of people living in the community served by the hospital.
Summit presentations included:
- Highlights of the the new legal provisions, especially the inclusion of “access to adequate nutrition” as a significant health need at the community level that can be addressed in the community benefit activities of tax-exempt hospitals. Inclusion of this language by the IRS in its Final Rule came about as a result of the many public comments received from community organizations across the country that witness the effects of hunger and food insecurity in communities every day.
- The “medicine” of food insecurity: how food insecurity causes and exacerbates many chronic diseases, by physician-researcher Dr. Seth Berkowitz from Harvard Medical School.
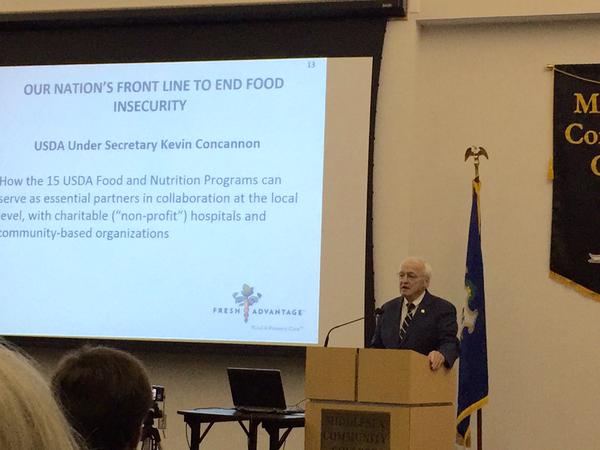
- The range of USDA food and nutrition programs—the frontline against hunger and insecurity in the U.S.— with which non-profit hospitals can collaborate to further strengthen their impact on food insecurity in the U.S., by Under Secretary Kevin Concannon, with specific examples from Cleveland Clinic, Arkansas Children’s Hospital, and other visionary hospitals.
- Examples of evaluation methodologies to demonstrate the impact of food system interventions such as mobile markets, by Dr. Kim Gans, University of Connecticut and Brown University. Evaluation plans and annual reporting of impact of specific activities and investments are required by the regulation.

- A case study of Hartford Hospital’s community benefit investment in a mobile market serving neighborhoods with the highest food insecurity rates, in one of Connecticut’s poorest urban centers by Kole Akindele, JD., Hartford Hospital and Martha Page, Hartford Food Systems.
The Connecticut Food Policy Council’s leadership in convening a forum that offered education and important networking opportunities provides a model for Food Solutions New England and food policy councils in our region to follow. The real potential of the ACA provision and IRS Final Rule that seek to strengthen the community benefit programs of tax-exempt hospitals needs concerted action at the local and state level whereby parties with resources, capacity and expertise can join together to get back to basics and bring nutritious food to all people. As is often said,
“Food is Medicine” and an avenue now exists for hospitals to play a role in making it so.
Presentations and all resource materials are available here.
Marydale DeBor, JD is Founder and Managing Director of Fresh Advantage® LLC, a consulting firm that is a pioneer in reframing how food and nutrition must be incorporated into all health care practices—from acute care environments to outpatient and community-based settings. The firm assists a wide variety of organizations in transforming institutional food service operations, combined with clinical and programmatic nutrition initiatives to promote health.




