
By Sandra Aronson, MS, MPH
The National Strategy: A Comprehensive Approach
The White House Conference on Hunger, Nutrition, and Health, held in September 2022, marked a significant milestone in the United States’ efforts to address diet-related diseases and health disparities. Fifty-three years after the first conference in 1969, the Biden administration announced a goal of ending hunger and increasing healthy eating and physical activity by 2030. The National Strategy, outlined in five pillars, focuses on improving food access and affordability, integrating nutrition and health, empowering consumers, supporting physical activity, and enhancing nutrition and food security research.
The strategy aims to address the social determinants of health that underlie many diet-related health challenges along the rural-urban continuum. While the strategy provides a federal roadmap for action, its success will ultimately depend on how well it is implemented at the community level. While all five pillars are important and deserving of further exploration and support, Food is Medicine interventions are gaining traction and present a unique opportunity to address the second pillar—integrating nutrition and health.
The Transformative Potential of Food is Medicine Interventions
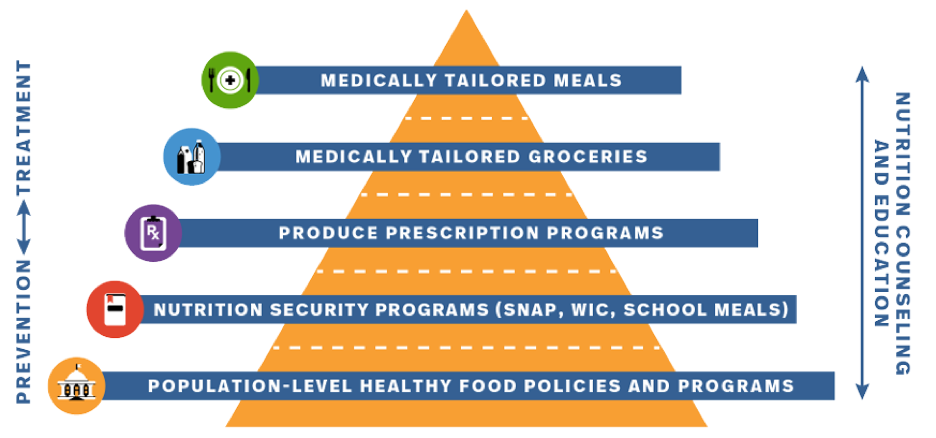
Figure adapted and updated from Food is Medicine Massachusetts (https://www.foodismedicinema.org/interventions-1)
Food is Medicine interventions, such as medically tailored meals and produce prescriptions, have shown promising results in improving health outcomes and reducing healthcare costs. A 2019 study on medically tailored meals and healthcare utilization by Community Servings estimated a 16 percent net reduction in average monthly healthcare costs for patients who received home-delivered medically tailored meals. This study also looked at studies conducted by Food Is Medicine Coalition (FIMC) members, who share that nutritional interventions resulted in a 63 percent reduction in hospitalizations, a 50 percent increase in medication adherence, and a 58 percent decrease in emergency department visits. By addressing the root causes of poor health through targeted nutrition support, these interventions have the potential to play a significant role in achieving the goals of the National Strategy.
However, scaling these interventions requires more than just policy change at the federal level. It demands a deep commitment to community engagement and a willingness to prioritize the lived experiences and expertise of those most impacted by diet-related health disparities.
Putting Communities at the Heart of Food is Medicine
The Bridging the Gap: Reducing Disparities in Diabetes Care initiative, which worked with health and social service organizations across the US to address the needs of patients with diabetes, identified four key strategies for increasing food access and reducing food insecurity in disadvantaged populations: embedding food distribution in clinical settings, tailoring interventions to address systemic barriers, bolstering local economic vitality, and advancing cross-sector collaboration. By implementing these strategies, community-based health care organizations are improving access to healthy food and creating the foundation for successful Food is Medicine interventions that can improve health outcomes and reduce disparities.
One organization demonstrating the power of community-driven Food is Medicine efforts is About Fresh, which started locally in Boston and has now expanded nationally through its Fresh Connect program. They embed community-driven advocacy into its model, engaging residents through their mobile markets, relying on local volunteers, partnering with community organizations, and remaining responsive to community needs as they grow. By starting with deep local roots and scaling strategically, About Fresh shows how community-based initiatives can grow their impact while maintaining community engagement as a core value.
Similarly, La Clínica del Pueblo in Washington, D.C., and Food & Friends have partnered with FRESHFARM to distribute culturally responsive food bags to immigrant clients. This collaboration addresses language and sociocultural barriers that may limit access to traditional food banks and pantries. It also supports local farmers and bolsters the local food system.
God’s Love We Deliver in New York City has also demonstrated the value of community engagement in Food is Medicine programs through initiatives like their client recipe project. By inviting clients to submit personal recipes for inclusion in a cookbook and potential adaptation for the organization’s menu, God’s Love We Deliver actively seeks and incorporates community perspectives, fostering a sense of ownership and empowerment that can enhance engagement retention and improve health outcomes.
These examples illustrate how community-based organizations are uniquely positioned to address food insecurity by leveraging their trusted relationships with patients, their deep understanding of local contexts and barriers, and their ability to forge partnerships across the health and social service sectors. By addressing the root causes of food insecurity, such as poverty, structural racism, and limited access to affordable, healthy food, these programs have the potential to create lasting, transformative change. As we seek to scale up food is medicine interventions and achieve the goals of the White House Conference on Hunger, Nutrition, and Health, we must ensure that community engagement remains at the forefront.
Best Practices for Community Engagement in Food is Medicine Programs
What does effective community engagement look like in practice? Some key best practices include:
- Partner with trusted community-based organizations and leaders who have deep roots and relationships within their communities.
- Conduct listening sessions, focus groups, and individual assessments to gather community input and insights into local needs, preferences, and barriers.
- Involve community members in program design, implementation, and evaluation to foster a sense of ownership and empowerment.
- Build mechanisms for ongoing feedback and adaptation to ensure programs remain responsive and accountable to the people they serve.
- Compensate community members for their time and expertise.
The best practices in Food is Medicine programs can be applied at various scales, from local to regional to national. At the local level, organizations like FreshRX in Tulsa, OK, and Community Servings in Boston, MA, work directly with communities to identify their unique needs and develop tailored interventions that address diet-related health challenges. Food is Medicine Massachusetts established a task force for program leaders and communities of practice to come to a consensus on standards for Food is Medicine interventions and definitions. It is also creating a Community Advisory Board to enhance community participation. Regionally, Food Solutions New England (FSNE) is advancing these best practices by convening diverse interest holders, facilitating dialogue, and fostering partnerships across the New England states. At the national level, organizations like the Food is Medicine Coalition (FIMC), and the Food is Medicine Institute work to advance policies and funding mechanisms that support the expansion of these programs while prioritizing community engagement and health equity. By leveraging the expertise, networks, and resources of organizations at all levels, we can support the development of effective, sustainable, and equitable food is medicine programs that improve health outcomes and reduce disparities.
Challenges and Barriers
While community engagement is essential for the success of food is medicine interventions, it is not without its challenges. One significant barrier is the lack of trust between communities and healthcare institutions, particularly in marginalized populations that have experienced historical discrimination and mistreatment. Building trust requires time, consistency, and a willingness to listen and respond to community concerns. Another challenge is the power imbalance between communities and institutions, making it difficult for community members to feel heard and valued in decision-making processes. Overcoming this barrier requires a commitment to shared power, leadership, and transparent and accountable communication. Limited resources and capacity can also hinder community engagement efforts, as organizations may struggle to allocate sufficient time, staff, and funding to build and maintain relationships with communities. Addressing this challenge requires creative partnerships, leveraging existing community assets, and advocating for dedicated resources to support community engagement. Despite these challenges, the benefits of authentic community engagement far outweigh the costs, and investing in these efforts is essential for creating equitable and sustainable change in food is medicine interventions.
Prioritizing Community Voices: Advancing the Strategy through Collaboration

Created by U.S. Department of Agriculture
The White House Conference on Hunger, Nutrition, and Health has provided a roadmap for transforming our food system and improving health outcomes for all Americans. However, to achieve these goals, we must prioritize genuine community engagement at every step. This means empowering community members to actively shape the programs and policies that impact their lives through collaborative partnerships. Community voices and priorities should be central to the process, from needs assessment and program design to implementation and evaluation. It’s also important to involve community representatives and advocates in decision-making bodies and governance structures.
Navigating complex policy levers and bureaucratic processes can be challenging for communities, so trusted community advisors, legislators, community health workers, and champions who understand local contexts and have lived experience are essential in helping communities navigate these complexities while ensuring that their perspectives and knowledge are represented and understood.
To advance the National Strategy through community-centered collaboration, policymakers, funders, healthcare providers, and community organizations must:
- Allocate resources for community outreach, engagement, and capacity-building
- Establish partnerships with community-based organizations and leaders to ensure interventions are culturally relevant and responsive
- Create opportunities for community members to participate in decision-making processes and program evaluation
- Embrace flexibility and adaptability in program design and implementation to allow for changes based on community input and evolving needs
Investing in authentic engagement and collaborative partnerships may require shifts in traditional power dynamics and funding models, but it is essential for achieving the bold goals of the National Strategy and ensuring that no community is left behind. By prioritizing community voices and working together across sectors and disciplines, we can create a more just, equitable, and sustainable food system that promotes health and well-being for all.
To learn about some of the organizations or partners in your area, check out the FIMC Partner Page.
To learn more about the use of food as medicine in the prevention, treatment, and management of disease, please see the Center for Food As Medicine website.
Former FSNE Program and Network Coordinator, Sandra remains passionate about scaling up Food is Medicine initiatives and maintains a strong interest in improving food access and sustainability. She’s eager to connect with others who share her enthusiasm. If you’re involved in innovative projects that expand the reach of sustainable nutrition-based interventions for improved health, please get in touch with her at sandra.b.aronson@gmail.com to share your experiences and discuss potential collaborations.




